Governmental and private payor audits are a routine event if you are a provider of healthcare goods and services and submit claims to payors for reimbursement. Audits by the Centers for Medicare and Medicaid Services ("CMS") related to fee-for-service claims are the most daunting of all because payors must face a five-tier appeals process.
The CMS appeals process consists of the following five levels of appeal:
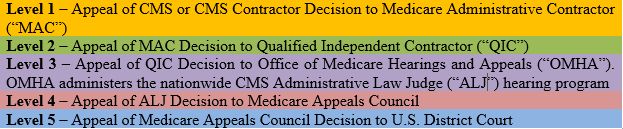
See MedLearn article on CMS appeals at https://www.cms.gov/outreach-and-education/medicare-learning-network-mln/mlnproducts/downloads/medicareappealsprocess.pdf and description of OMHA at https://www.hhs.gov/about/agencies/omha/index.html.
Effect of Reduction of ALJ Backlog and Possible Funding for QIC Opposition. When a provider reaches Level 3, the ALJ is required by statute to provide a hearing within ninety days of the provider's request. 42 U.S.C. §1395ff (d)(1)(A). However, during the last ten years, the ALJ has been extremely backlogged, resulting in providers waiting three to five years or more for a hearing at the ALJ. This is now changing, because between 2018 to the end of the first quarter of 2022, CMS has reduced the backlog by 88% (426,594 appeals down to 52,641), anticipating that it will clean up the backlog by the end of 2022. See https://www.aha.org/system/files/media/file/2022/03/aha-v-becerra-march-2022-status-repor-3-30-2t.pdf.
This means that the ALJ may soon be setting hearings in a timely manner, which could mean within 90 days of filing. In addition, the Department of Health and Human Services has submitted a budget request for FY 2022 that includes $6.2 million in funding to allow the QIC to participate as a party at the ALJ level. See https://www.cms.gov/files/document/fy2022-cms-congressional-justification-estimates-appropriations-committees.pdf at 143. If this measure is included in the 2022 budget, providers may see fast-moving appeals with active opposition by the QIC in the near future.
What can you do now to prepare for a possible fast-moving contested ALJ hearing? Here are our top three suggestions:
1. Prepare your initial document submission for an auditor's review. In many appeals, we see providers scrambling to pull together medical records and requested documentation in a hurried, jumbled manner. This makes sense, given the tight timeframes auditors provide for a response. However, the best defense is to think about what would help the auditor find your documentation and rule in your favor. This means adding organization and structure to your submission so that the auditor can easily locate supporting documentation. Consider organizing your documentation by type, in chronological order, and with an index or electronic links.
2. Choose your expert support early. The ALJ level is where an expert can really help a provider tell the story and support the claims from an overall clinical picture. Even so, we recommend bringing in the expert as early as possible. The expert can help oversee the submission of the original documentation, and can also help develop clinical strategies for upholding your claims. A small provider or provider with a low dollar amount at stake might be able to choose a physician or provider who either participated in the delivery of services in question or has an oversight role with the provider or provider entity to act as an expert. For larger appeals, a third-party expert with the right background can add the type of support that can win an appeal.
If the overpayment amount has been extrapolated, a statistical expert should also be retained early in the appeal process to review the extrapolation. CMS regulations require that certain criteria be utilized when determining an extrapolated overpayment, and if the MAC did not follow this criteria, arguments can be made to reduce the overpayment. If claims have been overturned before the ALJ level, a statistical expert can also make sure that the MAC has adjusted the overpayment accordingly.
3. Identify regulatory and legal arguments early. Hand-in-hand with the expert is the early identification of regulatory or legal arguments. Is the auditor over-reaching or applying the applicable regulatory framework incorrectly or inaccurately? Are there legal justifications that can help support your appeal? Getting an early start on this support can help start winning claims at the early levels, but also prepares providers well for the ALJ level.
In conclusion, it appears the ALJ may be back to holding hearings quickly, within 90 days of filing, as the historic backlog of claims is reduced. The ALJ level may also become more challenging if the QIC begins appearing more frequently as a party. To prepare, we recommend you act early in the audit process, by submitting well-organized documentation, adding a good expert(s) quickly, and developing the regulatory and legal arguments as soon as possible. In Medicare appeals, a quickly developed defense strategy can result in retaining more of your hard-earned reimbursement.
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.


