In June 2023, the Center for Medicare & Medicaid Innovation ("CMMI") at the Centers for Medicare & Medicaid Services ("CMS") released the Making Care Primary ("MCP") demonstration program – a 10.5-year, voluntary multi-payer model aimed at improving the quality of primary care and reducing overall health care spending.1 MCP launches on July 1, 2024 in an initial batch of eight states2 and creates a new pathway for organizations, particularly smaller primary care practices and Federally Qualified Health Centers ("FQHCs"), operating under a fee-for-service ("FFS") payment system to shift to a value-based payment model involving prospective, capitated payments. It will allow participants to receive funding and support to build a value-based care practice.
With the application window for participation in MCP now open until December 14, 2023, this article offers key context and considerations for potential participants and other stakeholders, especially as there are important impacts and tradeoffs regarding the ability to participate in the constellation of other innovative CMS health care payment models.
MCP Eligibility
For a provider to consider MCP participation, they must meet the strict eligibility criteria. Eligibility for MCP is based on the following criteria for participants:
- Established as a legal entity formed under applicable state, federal, or Tribal law authorized to conduct business in each state in which it operates;
- Medicare-enrolled;
- Bills for health services furnished to a minimum of 125 attributed Medicare beneficiaries;
- Has the majority (at least 51%) of their primary care sites (physical locations where care is delivered) located in an MCP state; and
- Is not a "concierge" medical practice, which is described to mean a practice that accepts patients who pay a membership fee up front.
Additionally, MCP participation will be determined at the organizational Taxpayer Identification Number ("TIN") level, as are many other CMMI programs.3 While each TIN must be its own participant and will be evaluated separately, FQHCs and Indian Health Programs can continue to work together in the model if desired. Organizations (at the TIN level) must meet the applicant eligibility requirements for their selected track.
MCP Objectives
MCP reflects CMS's goal of advancing health equity and acknowledging the critical role of primary care providers in identifying and addressing health-related social needs ("HRSNs") as a means of doing so.4 It builds on the recent effort by CMMI to expand the range of services covered under Medicare and Medicaid to include services addressing health-related social needs.5 MCP includes several model components designed to improve health equity.6 For example, participants will be required to develop health equity plans, and will receive additional payments to implement HRSN screening and referrals.
The focus on HRSN underscores the long-standing role of primary care providers as the first point of contact for most people within the health care system. MCP complements existing social service programs and other CMMI initiatives by expanding and incentivizing primary care engagement with patients. MCP also fits into CMS's overarching goal of shifting towards a payment system based on value and outcomes but adds to its prior initiatives a focus on primary care in underserved communities.
Intended participants are smaller practices, or unique practices like FQHCs, that generally do not have the attributed beneficiaries, or infrastructure or scale to participate in Accountable Care Organizations ("ACOs") or to assume considerable financial risk. Moreover, it provides those programs with the tools they need to address HRSNs, and improves their behavioral health capabilities, resulting in an overall positive impact to help achieve CMS's health equity goals.
MCP Structure7
MCP incentivizes primary care providers to transition away from traditional volume-based FFS payment. The overall design of MCP provides a gentle "on-ramp" for smaller, safety net primary care organizations to jump onto the bandwagon of value-based payment and care without having to participate in an ACO. To this end, MCP builds up the participants' infrastructure – through financial support and assistance creating partnerships – to prepare them to participate in other CMMI programs down the road. The design also provides tools to address the issues that primary care practices face in implementing and sustaining integrated behavioral health care through measurement-based care, utilizing evidence-based screening and evaluation tools and patient data to inform treatment decisions.8
MCP is organized in a three-track design, including six different payment structures that require participants to move through time-limited tracks over the model performance years, with increasing levels of accountability for cost and quality outcomes. Participants with no experience in value-based care must begin in the first track, while those with more experience can start in the second or third. The three progressive tracks are Building Infrastructure, Implementing Advanced Primary Care, and Optimizing Care and Partnerships. Participants must meet the care delivery requirements in their starting track by the end of Performance Year Two (December 31, 2025).
Payment Structure
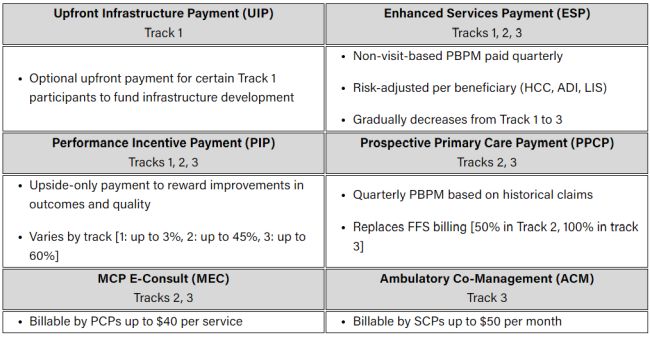
The model offers six payment mechanisms that CMS applies variably across the three model tracks.
Performance Incentive Payment ("PIP")
The PIP is an opportunity for an upside-only performance-based payment adjustment. Performance is evaluated through a list of quality, cost, and continuous improvement measures. The PIP is available to participants in each of the three tracks, with increasing payments in more advanced tracks:
Track 1: Up to 3% of the FFS payments made to the participant.
Track 2: Up to 45% of the total of FFS and prospective primary care payment ("PPCP") payments made to the participant, subject to participant scoring at least in the 30th percentile for the Total Per Capita Cost performance measure.
Track 3: Up to 60% of the total of FFS and PPCP payments made to the participant, subject to participant scoring at least in the 30th percentile for the Total Per Capita Cost performance measure.
Enhanced Services Payment ("ESP")
Another available payment is the ESP, which is a per-beneficiary per-month payment designed to compensate providers for the clinical and social risk associated with the provider's attributed population based on Medicare Part D low-income subsidy enrollment, the Area Deprivation Index, and the CMS-Hierarchical Condition Categories. This payment will be distributed prospectively on a quarterly basis, intended to fund ongoing care management activities.
The ESP is available to participants in each of the three tracks, with decreasing payments in more advanced tracks.
Upfront Infrastructure Payment ("UIP")
Eligible participants also are eligible to receive a time-limited, lump sum infrastructure payment (UIP). This is designed to provide start-up financial support is for health IT investments, such as connecting with health information exchanges ("HIEs"), e-consult technology investments, patient health data systems (i.e., patient portals), event notification systems, or electronic health record interfaces, which are not otherwise billable under Medicare FFS.
The UIP is only available to participants in Track 1.
Prospective Primary Care Payment ("PPCP")
Participants in Track 2 and Track 3 also are able to obtain a PPCP, a per-beneficiary per-month payment, paid quarterly on a prospective basis, based on historical claims for aligned beneficiaries. This payment replaces FFS billing in Track 2 (replaces 50% of claims payments) and Track 3 (replaces 100% of claims payments).
The PPCP is only available to participants in Track 2 and Track 3.
MCP e-Consult ("MEC")
Participants in Track 2 and Track 3 will be eligible to bill a new e-consult code that is unique to MCP. CMS has set a $40-per-service payment rate, which is designed to incentivize and encourage primary care clinicians to increase use of e-consults.
The MEC is only available to participants in Track 2 and Track 3.
Ambulatory Co-Management ("ACM")
The ACM is a unique payment for Track 3, which is designed to compensate specialty care partner physicians ("SCPs") who partner with participants for increased communication and collaboration with beneficiaries. Through this payment, SCPs will be eligible to bill a new short-term coordination code, which will allow SCPs to bill up to $50 per month.
The ACM is only available to participants in Track 3.
Table 1. MCP Payment Structures
Track 1: Building Infrastructure
Track Objectives
The first track is designed for participants with no experience in value-based care9 who are building the foundation to implement advanced primary care services through activities such as risk-stratifying their population, developing workflows for care management, chronic disease management, and behavioral health and HRSN screenings. Additionally, participants will develop workflows for chronic and episodic care management by leveraging CMS data to identify appropriate specialty care partners in the region.
Payment Structure
Track 1 participants generally will continue to receive reimbursement for care on an FFS basis with the addition of the UIP, ESP, and PIP payments.
Track 2: Implementing Advanced Primary Care
Track Objectives
In Track 2, participants continue to meet the requirements of Track 1 while also expanding and integrating the services available to their patients. In other words, once patients are risk-stratified and care management workflows are established, Track 2 involves implementing chronic and episodic care management and chronic condition self-management support services; implementing the practice's planned behavioral health integration approach; implementing social service referral workflows; systematically screening patients for behavioral health conditions; establishing partnerships with social service providers; and utilizing a community health worker ("CHW") (or equivalent staff) in supporting high-need beneficiaries.
Payment Structure
Track 2 shifts payment to 50% traditional FFS payments and 50% payments made through the ESP, PIP, PPCP, and MEC distributions.
Track 3: Optimizing Care and Partnerships
Track Objectives
In Track 3, participants will continue to meet and build upon the requirements of Tracks 1 and 2 to further enhance primary care services and expand care delivery and specialty care integration. Specifically, participants will offer individualized care plans, and expand chronic condition self-management support services to include group education and linkages to community-based supports. Participants will leverage the ACM payment to strengthen relationships with specialists and will optimize social service referral workflows, partnerships with social service providers, and the use of community health workers.
Payment Structure
Under Track 3, participants will be paid on a fully prospective basis using five payment mechanisms: ESP, PIP, PPCP, MEC, and ACM.
Detailed information on these track objectives and payment types along with other pertinent information is available within the Request for Applications ("RFA"), which CMS has recently made available for those who want to apply for MCP through December 14, 2023.10
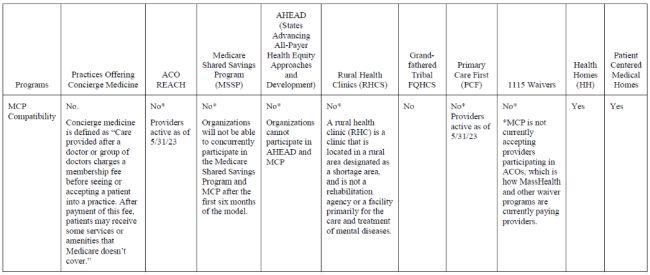
Comparison of MCP to Other Alternative Payment Models
MCP in the Context of Other Federal Initiatives
As currently designed, a significant consideration for potential participants is that MCP participation precludes participation in another CMS or CMMI programs impacting primary care delivery, including Rural Health Clinics; Primary Care First ("PCF") participants; ACO Realizing Equity, Access, and Community Health ("REACH") participants; the recently announced States Advancing All-Payer Health Equity Approaches and Development ("AHEAD") Model; and Grandfathered Tribal FQHCs. Additionally, primary care organizations will not be able to concurrently participate in the Medicare Shared Savings Program ("MSSP") and MCP after the first six months of the model.11
Primary care organizations, measured at the TIN level, will have to choose which CMMI program – ACO REACH, MSSP, AHEAD, or MCP – is best suited for their needs, especially given contractual and other commitments to these prior models. To the extent primary care organizations are already committed to another model and bound to that model for additional years, MCP may have limited impact. Additionally, larger primary care organizations are unlikely to have the necessary geographic footprint as 51% of their practice sites must be located in the eight MCP states. These features of MCP leave smaller primary care practices who are based in one or more MCP states most suited to avail themselves of the PCP program, particularly if they are not able to benefit from current ACO REACH or MSSP programs due to attribution requirements and other financial reasons such as downside risk and interest payment structures.12
MSSP. CMMI's Medicare Shared Savings Program ("MSSP") first encouraged a health care delivery system based on hospital and physician collaboration and value-based payment model through ACOs. Providers in MSSP are paid directly for each covered service received by a Medicaid beneficiary. MSSP participants who reduce costs below a benchmark and satisfy quality metrics may be rewarded through shared savings by satisfying four domains of quality measures.13 MSSP also gave participants a flexible system of various risk levels from which to choose depending on the circumstances and preferences of the participants.14 Unlike the ACO model, where participants continue to be reimbursed for each service, MCP aims to transition primary care providers from FFS reimbursement to prospective payments based on improving care and outcomes and reducing costs.15
ACO REACH. Other CMMI models, like the ACO REACH model, use a capitation-based payment system.16 Capitation systems provide health care providers and organizations with prospective payments designed to cover the predicted cost of all or some of the health care services for a specific patient over a certain period of time.17 ACO REACH provides two options for participants: one involves just primary care services and requires a lower-risk sharing arrangement (50% savings/losses); and another involves all health care services that an individual experiences in a year and requires a higher risk sharing arrangement (100% savings/losses).18 In contrast to ACO REACH, MCP allows participants to transition to prospective, capitated payments gradually and the eligibility criteria for participating is easier to meet.19 In addition, MCP allows smaller entities that want to participate in value-based care to do so independently, rather than as part of a larger ACO entity.
AHEAD. States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model. This newly introduced model targets historical underinvestment in primary care through statewide primary care investment targets. This model uses a flexible framework of care transformation activities to align with existing Medicaid value-based payment arrangements.20 Importantly, participants cannot participate in AHEAD within an MCP state.
All-Payor Pilots. MCP also builds upon lessons learned from Maryland's All-Payor Model (the first of its kind) and specifically its Care Redesign Program ("CRP"), implemented in 2017.21 Maryland's CRP Model allows hospitals to partner with and provide incentives and resources to certain Medicare-enrolled providers and suppliers.22 In return for these incentives and resources, providers and suppliers agree to perform activities and processes aimed at improving patient quality of care and reducing growth in the total cost of patient care.23 MCP incentivizes participants to engage similarly with specialty care clinicians and community-level support and services, and looks to achieve multi-payor alignment, but includes a scope of providers broader than just hospitals.24
MCP in the Context of Other State Initiatives
MCP appears to be more aligned with existing state-based initiatives focused on Medicare and Medicaid populations, as compared to the federal analysis above. Three state-based Medicaid programs are particularly salient: Patient Centered Medical Home ("PCMH"), Health Homes, and initiatives authorized under existing 1115 Waiver programs in some of the MCP states. What MCP is aiming to do is implement aspects of HRSN-focused care delivery present in these Medicaid programs into the delivery of Medicare programs.
1115 Waiver Programs. CMMI appears to be aligning the eight MCP states to states with existing or pending 1115 Medicaid Demonstration waivers, which, in large part, provide new funding streams for HRSN. As background, 1115 Medicaid Demonstration Waivers offer states the ability to deviate from federal statutes and implement their own approach to Medicaid delivery that will better serve the population. It generally reflects priorities identified by the states and the federal Centers for Medicare and Medicaid Services (CMS), as well as changing priorities from one presidential administration to another.25
For example, Massachusetts recently expanded their MassHealth Medicaid waiver program to test the efficacy of innovative practices aimed at promoting consistently high-quality, evidence-based, coordinated, and integrated care with the combined goals of providing medical assistance and improving the health of the communities served through the demonstration.26
Through the Flexible Services Program ("FSP"), MassHealth previously funded HRSN ventures through the Delivery System Reform Incentive Program, which functioned as a grant from CMS.27 The updated waiver for MassHealth28 shifts coverage of the FSP to managed care systems.29 Now, payments to state-based ACOs and MCOs that are a part of the state program will include risk adjustments related to social drivers of health. These risk adjustments mean that ACOs and MCOs receive higher payments to care for people with more significant HRSN.30
MCP and 1115 Waivers similarly aim to advance the health needs of populations that are not adequately served. Both programs aim to address HRSNs, but states with approved waivers can dictate the population focus and types of social supports provided. Given this overlap, it is likely that CMS and CMMI have been purposeful in launching MCP in states where there is already a robust or planned effort to fund HRSNs. Importantly, this connection between states with approved or pending 1115 waivers regarding HRSN and MCP designation gives participating practices the most meaningful opportunity to address social needs and make community connections.
Despite alignment of the programs, the payment structure of the two can lead to difficulties to providers looking to engage in both simultaneously. MCP is not currently accepting providers participating in ACOs, which is how MassHealth and other waiver programs are paying providers.
PCMH. The Patient-Centered Medical Home ("PCMH") program is focused on coordinating patient care across the health system, thus allowing delivery of higher quality and cost-effective care.31 PCMH programs pay providers an additional per-member per-month reimbursement to coordinate and manage the care of their patients. Providers also receive traditional FFS reimbursement for evaluation and management services as well as for the provision of items or procedures.32 To achieve PCMH recognition, practices must meet quality standards in six areas set by the National Committee for Quality Assurance.33
The current terms of MCP do not appear to exclude participation in PCMH models, suggesting that a practice can both qualify for funding under MCP and continue to receive their existing PCMH funding, which could be a beneficial source of funding given the similarity of the efforts involved.
Health Homes. The Health Homes Program is an optional Medicaid State Plan program for states to establish Health Homes to coordinate care for people with Medicaid who have chronic conditions.34 Health Homes providers integrate and coordinate all primary, acute, behavioral health, and long-term supports to treat the whole person. By focusing care coordination on those with the greatest needs, states can target a greater potential in improved health outcomes and savings.
States have flexibility in determining eligible providers for the program.35 Similarly, states also have flexibility in designing payment structures and receive a 90% Federal Medical Assistance Percentage ("FMAP") reimbursement rate to cover the federal share of most Medicaid expenditures and services under Section 2703.36, 37
Given the strong care coordination function already performed by Health Homes in many of the MCP states,38 it is not yet clear how eligible MCP primary care organizations will align with and not duplicate the care coordination efforts of Health Homes, which seemingly perform many of the same functions required of MCP-participating practices with a focus on mental and chronic conditions. While MCP could create another revenue stream for these primary care practices, it is possible that MCP could unintentionally create competing care management responsibilities and potential conflicts between Health Homes and MCP practices, if MCP does not account for this overlap in responsibilities.
Immediate Considerations for Stakeholders
With the December 14, 2023, application deadline rapidly approaching, providers will need to decide quickly whether to pursue MCP instead of other CMMI-related opportunities and understand how MCP may impact other programs in which they participate. Despite its similarities to prior CMS models and key state-based initiatives, MCP is distinct in its approach to improving primary health care by focusing on addressing health-related social needs. Its prospective, value-based payment system and partnerships between physicians and social workers and community-based support aim to improve primary care in conjunction with other federal and state efforts, such as under 1115 Medicaid Demonstration waivers.
To that end, MCP may be a promising program for applicants new to value-based payments, with its carefully designed progressive tracks, but may be constrained by limited eligibility (due to practices already participating in other CMMI programs) or operational conflict between other state-initiatives that may not have been appropriately accounted for in MCP's design. It is important that organizations considering participation carefully assess these tradeoffs and considerations before electing to participate in MCP.
MCP Eligibility Chart
CMS has provided further details about state-specific eligibility criteria for applicants in the Request for Applications (RFA).
Footnotes
1. "Making Care Primary (MCP) Model," Centers for Medicare and Medicaid Services, https://innovation.cms.gov/innovation-models/making-care-primary.
2. The eight states include Colorado, Massachusetts, Minnesota, New Jersey, New Mexico, New York (certain upstate counties), North Carolina and Washington.
3. MCP for Federally Qualified Health Centers and Indian Health Programs Overview Webinar Slides, Centers for Medicare and Medicaid Services, supra note 6 at Slide 18.
4. "Strategic Direction," Centers for Medicare and Medicaid Services. https://innovation.cms.gov/strategic-direction.
5. In December 2022, CMS released guidance for addressing HRSN through 1115 waivers, and in January 2023, CMS published guidance for allowing Medicaid-managed care plans to cover HRSNs; HRSNs are unmet social conditions, such as lack of housing or food insecurity, that contribute to poor health. Elizabeth Hinton, "A Look at Recent Medicaid Guidance to Address Social Determinants of Health and Health-Related Social Needs," Kaiser Family Foundation, February 22, 2023. https://www.kff.org/policy-watch/a-look-at-recent-medicaid-guidance-to-address-social-determinants-of-health-and-health-related-social-needs/.
6. "Making Care Primary (MCP) Model," supra note 2.
7. All information in this section is compiled from the Making Care Primary Request for Applications Version: 1, and may be subject to change as the program evolves. See Making Care Primary Request for Applications Version: 1 https://www.cms.gov/files/document/mcp-rfa.pdf .
8. Nathaniel Counts & Celli Horstman, Making Care Primary: An Important Advance for Integrated Behavioral Health Care, The Commonwealth Fund, Aug. 18, 2023. https://www.commonwealthfund.org/blog/2023/making-care-primary-integrated-behavioral-health-care; see also Making Care Primary Request for Applications Version: 1.
9. Experience in value-based care is defined as participation in performance-based Medicare initiatives (including Primary Care First ("PCF"), Comprehensive Primary Care Plus "(CPC+"), Next Generation AGO ("NGACO"), Direct Contracting, Accountable Care Organizations Realizing Equity Access and Community Health ("ACO REACH"), and/or has been part of a Medicare Shared Savings Program ("SSP") ACO that has not deferred its entry into a second agreement period under a two-sided model under § 425.200(e) in the five most recent performance years prior to the start of the agreement. This includes scenarios where 60% or more of the TIN's NPIs or CCNs meet the aforementioned criteria.
10. Making Care Primary Request for Applications Version: 1 https://www.cms.gov/files/document/mcp-rfa.pdf.
11. "Making Care Primary (MCP) Model," supra note 4.
12. Rachel E. Yount, CMS Announces Changes to the MSSP Designed to Increase MSSP Participation and Promote Equity within the MSSP, Mintz, (November 17, 2022). https://www.mintz.com/insights-center/viewpoints/2146/2022-11-17-cms-announces-changes-mssp-designed-increase-mssp.
13. For more information on specific quality measures and performance standards, see https://www.cdc.gov/cliac/docs/addenda/cliac0212/Tab_22_November_CLIAC_2012Feb15_ACO_Overview_Final_Rule.pdf.
14. "Comparison of BASIC track and ENHANCED track," Medicare Shared Savings Program, March 2023. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/ssp-aco-participation-options.pdf.
15. "About the Program," Centers for Medicare & Medicaid Services. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/about (Last updated Sept. 6, 2023).
16. "ACO REACH," Centers for Medicare and Medicaid Services. https://innovation.cms.gov/innovation-models/aco-reach.
17. "Capitation and Pre-payment," Centers for Medicare & Medicaid Services. https://www.cms.gov/priorities/innovation/key-concepts/capitation-and-pre-payment.
18. The "Professional" arrangement provides one payment option for participants that comprises a risk-adjusted monthly payment for primary care servicers, the "Primary Care Capitation Payment." The "Global" arrangement includes the Primary Care Capitation Payment option as well as a risk-adjusted monthly payment for all covered services, including specialty care, the "Total Care Capitation Payment."
19. Unlike the ACO REACH, MCP does not have requirements regarding doctor-provider governance control. "Making Care Primary (MCP) Model," supra note 4.
20. "States Advancing All-Payer Health Equity Approaches and Development (AHEAD) Model", Centers for Medicare & Medicaid Services https://www.cms.gov/priorities/innovation/innovation-models/ahead
21. "Maryland All-Payer Model," Centers for Medicare & Medicaid Services. https://innovation.cms.gov/innovation-models/maryland-all-payer-model.
22. "Under each CRP Track, participating hospitals entered into financial arrangements with providers and suppliers that were enrolled in Medicare, provided items and services to Maryland Medicare beneficiaries, met additional qualifications specific to that CRP Track, and were approved by CMS ("Care Partners"). Under the terms of such financial arrangements, or "Care Partner Arrangements," the Care Partner received Incentive Payments, nonmonetary remuneration ("Intervention Resources"), or both; from the participating hospital in exchange for their performance of CRP Track-specific activities and processes ("CRP Interventions")." Id.
23. Id.
24. "Making Care Primary (MCP) Model," supra note 4.
25. "Medicaid Waiver Tracker: Approved and Pending Section 1115 Waivers by State," Kaiser Family Foundation, 2023. https://www.kff.org/medicaid/issue-brief/medicaid-waiver-tracker-approved-and-pending-section-1115-waivers-by-state/.
26. Administrator for the Centers for Medicare and Medicaid Services, Chiquita Brooks-LaSure to Assistant Secretary, MassHealth Amanda Cassel Kraft, September 28, 2022. Department of Health & Human Services. https://www.mass.gov/doc/masshealth-extension-approval/download.
27. Robert W. Seifert, "The MassHealth Demonstration Extension 2022–2027: Building on Success, Focusing on Equity," https://www.bluecrossmafoundation.org/sites/g/files/csphws2101/files/2023-06/MH_Demonstration_2023_FINAL_2.pdf.
28. Waiver is in place from October 1, 2022 through December 31, 2027.
29. Angela D. Garner, "MassHealth Technical Correction Approval Letter," https://www.medicaid.gov/medicaid/section-1115-demonstrations/downloads/ma-masshealth-ca-11072022.pdf.
30. Id. at 29.
31. "Patient-Centered Medical Home (PCMH) Model," Centers for Disease Control and Prevention. https://www.cdc.gov/dhdsp/policy_resources/pcmh.htm (Last updated May 12, 2021).
32. "Frequently Asked Questions: Patient Centered Medical Homes," New York State Department of Health, https://www.health.ny.gov/technology/innovation_plan_initiative/pcmh/faqs.htm.
33. The standard includes (1) team-based care and practice organization, (2) care management and support, (3) know and manage patients, (4) care coordination and care 34. transitions, (5) patient-centered access and continuity, and (6) performance measurement and quality improvement. "Patient-Centered Medical Home Recognition," National Committee for Quality Assurance (NCQA), https://www.ncqa.org/employers/ncqa-programs-of-interest-to-employers/patient-centered-medical-home-recognition/.
34. "Health Homes," Medicaid. https://www.medicaid.gov/medicaid/long-term-services-supports/health-homes/index.html.
35. Id. Providers can be (1) a health team comprising medical specialists, nurses, nutritionists, etc., (2) a team of health professionals, or (3) a designated provider such as a physician, group practice, community health center, etc.
36. Id.; "Medicaid's Federal Medical Assistance Percentage (FMAP)," Congressional Research Service, https://sgp.fas.org/crs/misc/R43847.pdf.
37. The health home services include comprehensive care management, care coordination, health promotion, comprehensive transitional care/follow-up, patient and family support, and referral to community and social support services. https://www.medicaid.gov/state-resource-center/medicaid-state-technical-assistance/health-home-information-resource-center/downloads/health-homes-faq-5-3-12_2.pdf.
38. Of the eight states, the following have a Health Home program: Colorado, Minnesota, New Mexico, New York, and Washington.
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.





