The Transparency in Coverage final rule, applicable to commercial insurers and effective July 2022, follows the Hospital Price Transparency rule by 18 months.1 Per the Centers for Medicare & Medicaid Services (CMS), the Transparency in Coverage final rule:
- Enables consumers to evaluate health care options and to make cost-conscious decisions
- Strengthens the support consumers receive from stakeholders that help protect and engage consumers
- Reduces potential surprises in relation to individual consumers' out-of-pocket costs for health care services
- Creates a competitive dynamic that may narrow price dispersion for the same items and services in the same health care markets; and
- Puts downward pressure on prices which, in turn, potentially lowers overall health care costs.2
Additional requirements will go into effect on January 1, 2023, and January 1, 2024.3 The Hospital Price Transparency rule focuses on payer-specific negotiated charges, whereas the Transparency in Coverage rule provides an estimate of the individual's cost-sharing liability. Machine-readable files must include rates for all covered items and services between the plan or issuer and in-network providers; allowed amounts for, and billed charges from, out-of-network providers; and negotiated rates and historical net prices for covered prescription drugs.4 Machine-readable files are required as of July 1, 2022.5 An internet-based self-service price comparison tool is required to generate cost-sharing estimates for 500 items and services effective January 1, 2023, and for all items and services one year later.6
Price Transparency Comparative Analysis
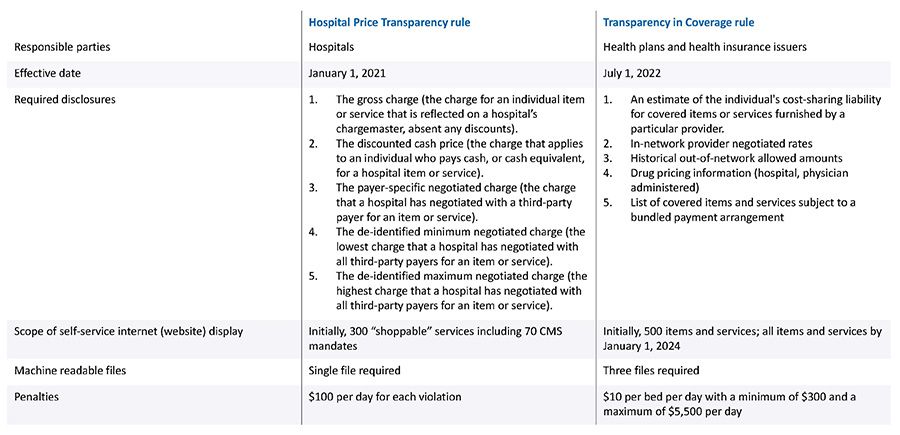
Source: https://www.federalregister.gov/documents/2020/11/12/2020-24591/transparency-in-coverage#h-11
The importance of price transparency cannot be overstated, as a wide disparity in procedural prices exists among hospitals located within a metropolitan statistical area (MSA), as well as within the same hospital among different payers and within a specific payer, by plan.
In terms of price variation across MSAs, the New York MSA has the highest average prices for joint replacement surgery at $58,193, more than double the price in St. Louis and Baltimore. The range of prices [for joint replacements] in the New York MSA is exceedingly broad, ranging from $44,597 to $70,610, thereby highlighting the importance of price transparency and the potential for "shopping around," assuming no difference in the quality of outcomes.7
Average Allowed Charges for In-Network Joint Replacement in Large Employer Plans by MSA

Source: https://www.healthsystemtracker.org/brief/price-transparency-and-variation-in-u-s-health-services/
Price distribution within a hospital by health plan and product type is also potentially broad.8 In general, Managed Medicaid rates are lowest, followed by Medicare Advantage and private insurance, the latter with a range of pricing based on negotiated prices by insurance carriers and health plans.9
Bottom Line:
Insurers are required to comply with the law. Price transparency will highlight disparities in price without necessarily justifying premium prices; re-negotiation may be warranted. Evidence of a relationship between cost and quality is low to moderate, regardless of direction.10 Higher out-of-pocket costs combined with rising consumerism increase the likelihood that patients will make cost comparisons, though data complexity may limit effectiveness.
Footnotes
1. Hospital Price Transparency. CMS.gov (last visited September 20, 2022). https://www.cms.gov/hospital-price-transparency
2. Federal Register, November 12, 2020. https://www.federalregister.gov/documents/2020/11/12/2020-24591/transparency-in-coverage#h-11
3. CMS.gov Transparency in Coverage (last visited September 6, 2022). https://www.cms.gov/healthplan-price-transparency
4. FAQS About Affordable Care Act Implementation Part 53 (April 19, 2022). https://www.cms.gov/files/document/faq-part-53.pdf
5. Carlton Pilger, Fisher Phillips. "July 1 Deadline Looming for Health Plan Transparency Disclosures." SHRM (June 22, 2022). https://www.shrm.org/resourcesandtools/hr-topics/benefits/pages/july-1-deadline-looming-for-health-plan-transparency-disclosures.aspx
6. Transparency in Coverage Rule. United Healthcare (last visited September 6, 2022). https://www.uhc.com/united-for-reform/health-reform-provisions/transparency-in-coverage-rule
7. "Price Transparency and Variation in U.S. Health Services." Peterson-KFF Health System Tracker (January 13, 2021). https://www.healthsystemtracker.org/brief/price-transparency-and-variation-in-u-s-health-services/
8. Ibid.
9. "Early results from federal price transparency rule show difficulty in estimating the cost of care." Peterson-KFF Health System Tracker (April 9, 2021). https://www.healthsystemtracker.org/brief/early-results-from-federal-price-transparency-rule-show-difficultly-in-estimating-the-cost-of-care/
10. "The Association Between Health Care Quality and Cost: A Systematic Review." Annals of Internal Medicine (January 1, 2013).
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.


