Introduction
Most health plans participating in either Medicaid/CHIP managed care programs (42 CFR 440.395) or Group Health Insurance markets (45 CFR 146.136) are required by the Centers for Medicare and Medicaid Services ("CMS") and/or the U.S. Department of Labor ("DOL"), to demonstrate and maintain compliance with The Mental Health Parity and Addiction Equity Act of 2008 ("MHPAEA"). These rules apply to all health coverage in the individual, small and large group insurance markets as well as to all private employer-sponsored plans (insured and self-insured), with certain exceptions.
As states and the federal government have started to take a closer look at compliance and associated enforcement activities, it is imperative that health plans take a hard look at parity compliance and address internal and external operations and policies to maintain compliance and execute comparative analyses as required by regulators.
This article provides a brief overview of mental health in the United States, some background of the rule, a snapshot into recent enforcement activities, a summary of specific areas where plans typically fall short and a high-level road map to improve operations and associated policies to address MHPAEA head-on.
Mental Health in the United States
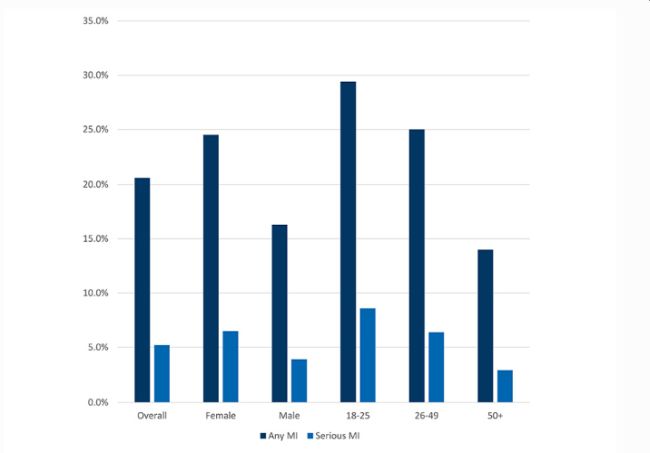
With 52.9 million adult Americans, which is 21.0 percent of the adult population, having any mental illness ("AMI"), and 14.2 million adults, which is 5.6 percent, having serious mental illness ("SMI"), the United States is facing a mental health crisis.1 Prevalence is higher in females than males, and in those <50 years.2 Less than half of adults with any mental illness received treatment.3 The rise in mental illness reflects increased awareness, declining stigmatization, and the impact of COVID-19. Drug overdose deaths have continued their inexorable rise driven by the opioid crises, i.e., fentanyl. More than 40 million Americans had a substance abuse disorder in 2020, many with a comorbid mental health issue.4 These statistics belie the importance of mental health and substance use disorder treatment, and regulators' focus on access and the delivery of mental health services.
Behavioral Health Epidemiology
Any mental illness (AMI) is defined as a mental, behavioral, or emotional disorder. Serious mental illness (SMI) is a mental behavioral or emotional disorder resulting in serious functional impairment interfering with or limiting major life activities.
Prevalence of Any and Serious Mental Illness, 2019
Drug Overdose Deaths, 2011-2021
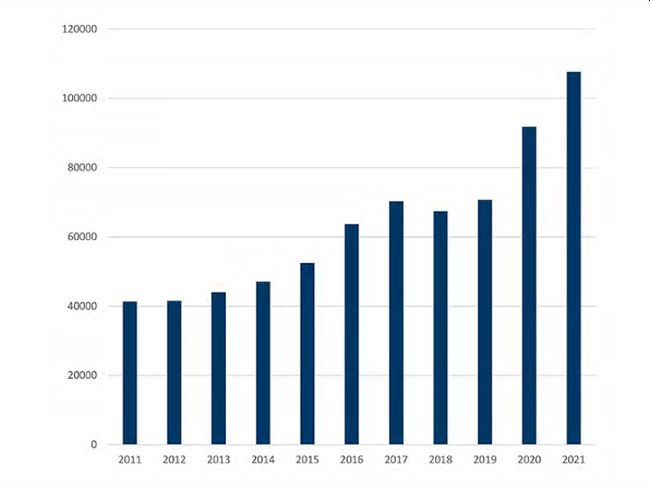
Source: National Institute of Mental Health, Drugs Most Frequently Involved in Drug Overdose Deaths: United States, 2011-2016, National Vital Statistics Report; Overdose death rates, National Institute on Drug Abuse 1999-2020
Does Mental Health Parity Apply to You?
Mental Health parity regulations apply to you (with certain exceptions) if your plan meets one of the following types:
- Medicaid Managed Care Plans: Managed Care Plans, PIHPS, PAHPS, ABP)
- CHIP
- Private Employer-Sponsored Group Health Plans: Self-Insured, Insured
- State and Local Government Employer Sponsored Health Plans: Self-Insured, Insured
- Individual Insurance Plans
- Small Group Insurance Plans
- Mental Health Parity does not apply in whole or in part to the following plan: Medicare, fee-for-service Medicaid, employer sponsored plans that received an exemption based on increase of costs related to parity and some state/local government employee health plans.5
Mental Health Parity Regulatory Timeline and Pending Changes
Initial parity regulations were introduced with The Mental Health Parity Act of 1996 ("MHPA") requiring that "large group health plans cannot impose annual or lifetime dollar limits on mental health benefits that are less favorable than any such limits imposed on medical/surgical benefits."6
In 2008, the scope of parity regulations was expanded for group health plans under the current law, The Mental Health Parity and Addiction Equity Act of 2008 ("MHPAEA"), which expanded protections for financial requirements and introduced protections for nonquantitative treatment limitations.7 In 2010 the Affordable Care Act ("ACA") extended parity to individual and small group markets along with other provisions, mandated BH coverage as an essential health benefit and eliminated the pre-existing condition clause preventing those with MH/SUD from receiving treatment.8
In 2013, the final parity rule for commercial plans was issued, and in 2016 the final Medicaid/CHIP parity rule was issued.9,10 Also in 2016, Congress passed the 21st Century Cures Act, which required agencies to provide more guidance related to Non-quantitative Treatment Limitations ("NQTL"s) testing and to increase enforcement activities.11 In 2020, Congress passed the Consolidated Appropriations Act ("CAA"), which required plans to conduct comparative analyses for regulators.12
Since that time, enforcement activities have begun to materialize, and the first federal parity lawsuit was brought by the NY Attorney General for NQTL violations.13 Reporting14 indicates that federal agencies and Congress may be updating parity regulations with the most significant reforms since the 2016 Medicaid/CHIP rule for the 25-year-old regulation.15
Our experience supporting plans and government agencies over the past decade tells us that requirements may streamline or increase (i.e., network adequacy, medical management criteria), but fundamental regulatory provisions are likely to remain, and plan operations should be structured to alleviate the conducting of required comparative analyses and compliance verification as needed and on an ongoing basis.
MHPAEA Top Enforcement Priority
On January 25, 2022, the U.S. Departments of Labor, Health and Human Services and the Treasury issued a report showing "failures to deliver parity in mental health, substance-use disorder benefits."16 The report also emphasizes increased MHPAEA enforcement by federal agencies. An enforcement tool - a comparative analysis of such NQTLs as medical management, step therapy and prior authorizations - was mandated for all plans in the CAA.17 Key enforcement activities include:18
The Employee Benefits Security Administration ("EBSA") within the Department of Labor has enforcement authority over group health plans with 136.5 million members
- "Issued 156 letters to plans and issuers requesting comparative analyses for 216 unique NQTLs across 86 investigations.
- Issued 30 initial determination letters finding 48 NQTLs imposed on MH/SUD benefits lacking parity with medical/surgical benefits.
- Received corrective action plans from 19 plans in response to initial determination letters."
CMS has enforcement authority in the individual and fully insured group markets in certain states and over non-federal governmental group health plans in all states
- "The EBSA has issued 156 letters to plans and issuers requesting comparative analyses for 216 unique NQTLs across 86 investigations.19
- Issued 15 letters between May and November 2021 to issuers in states where CMS has direct enforcement authority over MHPAEA (Texas, Missouri and Wyoming) and to non-Federal governmental plan sponsors in those and other states.20
- Issued 15 initial determination letters to plans and issuers finding 16 NQTLs out of parity with medical/surgical benefits.21
- Received corrective action plans from 6 plans and issuers in response to initial determination letters."22
Given the backdrop of the pandemic, access and limits imposed on MH/SUD services are under the microscope. State agencies have focused audit and compliance activities on MHPAEA compliance and have filed lawsuits or fined plans with required remediation corrective actions.
Here are several cases taken against organizations:
- The NY Attorney General made a $13.6 million payout to consumers who were denied outpatient psychotherapy by UnitedHealthcare.23
- The NY Attorney General determined that MVP violated parity laws by imposing stricter utilization review for behavioral health services; the state required specific remediation activities and fined the plan $300,000.24
- The NY Attorney General determined that Emblem Health violated parity laws by imposing stricter utilization review for behavioral health services; the state required specific remediation activities and fined the plan $1.2 million.25
- The NY Attorney General determined that Beacon Health Options violated parity laws, the state required specific remediation activities and fined the plan $900,000.26
- The Pennsylvania Department of Insurance fined UMPC Health Coverage, Inc. and UPMC Health Options, Inc. $250,000 and required corrective action following the department's audit findings in response to claims denials and processing delays.27
- The Pennsylvania Department of Insurance fined Aetna $190,000 and required corrective action following the department's audit findings due to violating rules on coverage of drug- and alcohol-abuse treatment and autism.28
- The California Department of Managed Health Care required the Kaiser Foundation Health Plan, Inc. to correct identified issues with the plan's oversight of and access to behavioral health services with a potential fine of $1 million.29
- The Illinois Department of Insurance fined five health plans for parity violations for an overall value more than $2 million. Plans fined include CIGNA Healthcare of Illinois ($582,000), UnitedHealthcare ($550,000), CIGNA Health and Life ($418,000), Health Care Service Corporation ($325,000) and Celtic ($208,000).30
- The Oregon Department of Consumer and Business Services issued fines to BlueCross BlueShield of Oregon ($100,000), UnitedHealthcare ($110,000), Kaiser Foundation Health Plan of Northwest ($250,000) and Pioneer Educators Health Trust ($100,000) for parity non-compliance.31
Where Organizations Fall Short
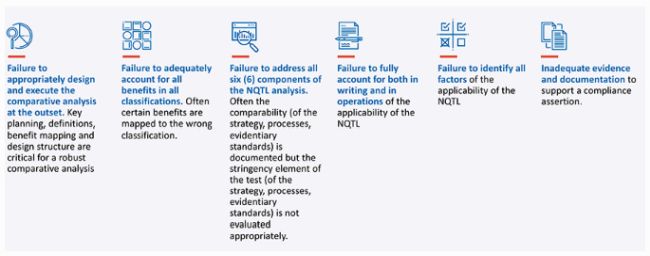
Over the years, we have refined our approach to MHPAEA compliance to anticipate where plans tend to fall short when completing the comparative analysis and continue to update our approaches to explain and acquire the needed information for a robust comparative analysis.
In our experience, organizations without appropriate training, dedicated efforts and resources typically fall short in their comparative analyses in the following ways:
FTI Consulting's Approach to Preparing, Testing and Streamlining Operations
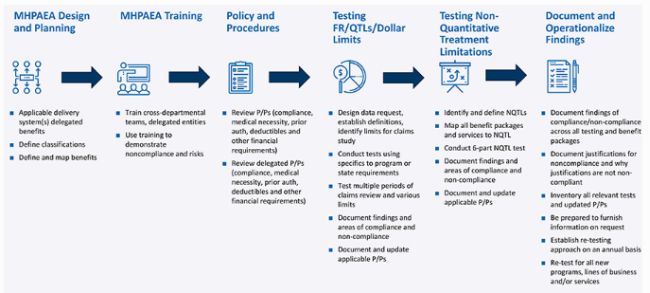
MHPAEA requirements are not going away, and organizations should consider oversight, compliance and reporting operations to reduce future administrative burdens while demonstrating parity. While CMS and DOL regulations do differ in certain ways, a fundamental streamlined compliance and testing structure can be very beneficial to organizations participating in these programs to address foreseeable reporting and compliance needs.
Over the past decade, we have learned a lot through helping clients (i.e., plans and government) test and achieve compliance with parity and have updated our approach to reflect up-to-date regulations and findings in recent reports from DOJ, CMS, and DOL. Our experience with end-to-end MHPAEA includes study design, trainings, evaluations, testing and analysis for all elements of the rule.
In our experience, every organization should consider the core study-, design- and operational steps when addressing state or federal requests for parity reports, when moving into a new market or when the plan looks to address internal operations for future parity compliance activities and audits. Below is an essential basic plan outline to consider when addressing parity:
 >
>
Final Thoughts
Organizations that look to address MHPAEA compliance across markets today will lead to a reduction in follow-up enforcement activities, saving organizations money and unwanted public attention. The rule is not going away. Address it head-on today instead of doing catch-up activities tomorrow.
Footnotes
1. "Mental Illness," National Institute of Mental Health (last updated January 2022), https://www.nimh.nih.gov/health/statistics/mental-illness#.
2. "Mental Illness." National Institute of Mental Health. (last visited December 7, 2022). https://www.nimh.nih.gov/health/statistics/mental-illness
3. "The State of Mental Health in America." Mental Health America. (last visited December 7, 2022). https://mhanational.org/issues/state-mental-health-america
4. "Highlights for the 2020 National Survey on Drug Use and Health," Substance Abuse and Mental Health Services Administration (last visited June 16, 2022), https://www.samhsa.gov/data/sites/default/files/2021-10/2020_NSDUH_Highlights.pdf.
5. "2022 MHPAEA Report to Congress. Realizing Parity, Reducing Stigma, and Raising Awareness: Increasing Access to Mental Health and Substance Use Disorder Coverage," Department of Labor, Department of Health & Human Services, and Department of the Treasury (2022), https://www.dol.gov/sites/dolgov/files/EBSA/laws-and-regulations/laws/mental-health-parity/report-to-congress-2022-realizing-parity-reducing-stigma-and-raising-awareness.pdf
6. "The Mental Health Parity and Addiction Equity Act (MHPAEA)," Centers for Medicare & Medicaid Services (last visited June 16, 2022), https://www.cms.gov/CCIIO/Programs-and-Initiatives/Other-Insurance-Protections/mhpaea_factsheet#.
7. Ibid.
8. "Compilation of Patient Protection and Affordable Care Act, As Amended Through May 1, 2010," Office of the Legislative Counsel; U.S. House of Representatives, 111th Congress, Second Session (May 2010), http://housedocs.house.gov/energycommerce/ppacacon.pdf.
9. Final Rules Under the Paul Wellstone and Pete Domenici Mental Health Parity and Addiction Equity Act of 2008; Technical Amendment to External Review for Multi-State Plan Program. Federal Register. (November 13, 2013) https://www.federalregister.gov/documents/2013/11/13/2013-27086/final-rules-under-the-paul-wellstone-and-pete-domenici-mental-health-parity-and-addiction-equity-act
10. Medicaid and Children's Health Insurance Programs; Mental Health Parity and Addiction Equity Act of 2008; the Application of Mental Health Parity Requirements to Coverage Offered by Medicaid Managed Care Organizations, the Children's Health Insurance Program (CHIP), and Alternative Benefit Plans. (March 30, 2016) https://www.federalregister.gov/documents/2016/03/30/2016-06876/medicaid-and-childrens-health-insurance-programs-mental-health-parity-and-addiction-equity-act-of
11. 21st Century Cures Act, Pub. L. No. 114-255, 130 Stat. 1033 (December 13, 2016), https://www.congress.gov/114/plaws/publ255/PLAW-114publ255.pdf.
12. Consolidated Appropriations Act, 2021, H.R. 133, 116th Congress. (2020) https://www.congress.gov/bill/116th-congress/house-bill/133/text.
13. "Mental Health Parity Update: DOL and NY AG Actions Highlight Ongoing Scrutiny of NQTLs." Manatt. (September 14, 2021) https://www.manatt.com/insights/newsletters/health-highlights/mental-health-parity-update-dol-and-ny-ag-actions
14. Kaye Pestaina, "Mental Health Parity at a Crossroads," Kaiser Family Foundation (August 18, 2022), https://www.kff.org/private-insurance/issue-brief/mental-health-parity-at-a-crossroads/.
15. Kaye Pestaina, "Mental Health Parity at a Crossroads - Appendix," Kaiser Family Foundation (August 18, 2022), https://www.kff.org/report-section/mental-health-parity-at-a-crossroads-appendix/.
16. "U.S. Departments of Labor, Health and Human Services, Treasury issue 2022 Mental Health Parity and Addiction Equity Act Report to Congress," U.S. Department of Health & Human Services (January 25, 2022), https://www.hhs.gov/about/news/2022/01/25/us-dol-hhs-treasury-issue-2022-mental-health-parity-addiction-equity-act-report-to-congress.html.
17. "2022 MHPAEA Report to Congress. Realizing Parity, Reducing Stigma, and Raising Awareness: Increasing Access to Mental Health and Substance Use Disorder Coverage," Department of Labor, Department of Health & Human Services, and Department of the Treasury (2022), https://www.dol.gov/sites/dolgov/files/EBSA/laws-and-regulations/laws/mental-health-parity/report-to-congress-2022-realizing-parity-reducing-stigma-and-raising-awareness.pdf.
18. Ibid.
19. Ibid.
20. Ibid.
21. Ibid.
22. Ibid.
23. "Attorney General James Provides $13.6 Million to Consumers Who Were Denied Mental Health Coverage," New York State Office of the Attorney General – Letitia James, NY Attorney General, (May 20, 2022), https://ag.ny.gov/press-release/2022/attorney-general-james-provides-136-million-consumers-who-were-denied-mental.
24. "Mental Health Parity: Enforcement by the New York State Office of the Attorney General," Health Care Bureau – New York State Office of the Attorney General (May 2018), https://ag.ny.gov/sites/default/files/hcb_mental_health_parity_report.pdf.
25. Ibid.
26.3 Ibid.
27. "Insurance Department Exam Finds UPMC Violations," Pennsylvania Pressroom, (December 30, 2021), https://www.media.pa.gov/pages/insurance-details.aspx?newsid=468.
28. "Commonwealth of Pennsylvania Insurance Department Market Conduct Examination Report of Aetna Health Insurance Company." (November 5, 2018) https://www.insurance.pa.gov/Regulations/Regulatory%20Actions/Documents/Current%20Market%20Conduct/Aetna_FinalExamReport_01042019.pdf
29. Jenny Gold. "Settlement Reached on Kaiser Permanente's Repeated Mental Health Care Deficiencies." California Healthline. July 19, 2017 https://californiahealthline.org/news/settlement-reached-on-kaiser-permanentes-repeated-mental-health-care-deficiencies/
30. "Pritzker Administration Announces Over $2 million in Fines for Major Health Insurance Companies Violating Illinois Mental Health Parity Laws," Illinois Department of Insurance (July 15, 2020), https://www2.illinois.gov/IISNews/21819-IDOI_Press_Release.pdf.
31. Morgan Haefner. "4 Oregon insurers face up to $250k fines for alleged mental healthcare violations." Becker's Payer Issues. (March 3, 2017) https://www.beckerspayer.com/payer/4-oregon-insurers-face-up-to-250k-fines-for-alleged-mental-healthcare-violations.html?utm_campaign=bhr&utm_source=website&utm_content=related
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.


