The American Heart Association (AHA) Scientific Sessions 2017, was a global event held from November 11-15, 2017 at California, USA. AHA's Scientific Sessions attracts nearly 18,000 attendees, with a global presence from more than 100 countries. In addition, two million medical professionals participate virtually in lectures and discussions about basic, translational, clinical and population science. Major landmark clinical trials and policy guidance in the domain of cardiology are presented at the AHA scientific sessions.
Some of the major clinical trials/policy statements from this year's AHA sessions are briefly discussed in this news report:
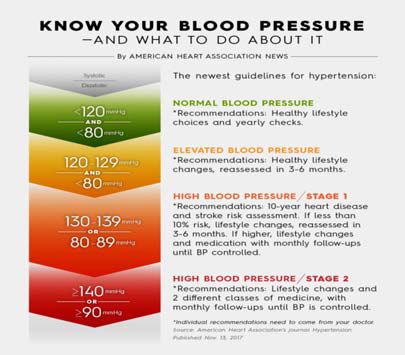
1. High blood pressure redefined for first time in 14 years: 130/80 mm Hg is the new high in the revised guideline
High blood pressure should be treated earlier with lifestyle changes and in some patients with medication – at 130/80 mm Hg rather than 140/90 mm Hg – according to the first comprehensive new high blood pressure guidelines in more than a decade. The guidelines are published by the American Heart Association (AHA) and the American College of Cardiology (ACC) for detection, prevention, management and treatment of high blood pressure20.
As against 1 in 3 U.S. adults having high blood pressure (32 percent) with the previous definition, the new guidelines will result in nearly half of the U.S. adult population (46 percent) having high blood pressure, or hypertension.
These guidelines, the first update to offer comprehensive guidance to doctors on managing adults with high blood pressure since 2003, are designed to help people address the potentially deadly condition much earlier.
The new guidelines also stress the importance of using proper technique to measure blood pressure. Blood pressure levels should be based on an average of two to three readings on at least two different occasions.
Blood pressure categories in the new guideline are:
- Normal: Less than 120/80 mm Hg;
- Elevated: Top number (systolic) between 120-129 and bottom number (diastolic) less than 80;
- Stage 1: Systolic between 130-139 or diastolic between 80-89;
- Stage 2: Systolic at least 140 or diastolic at least 90 mm Hg;
- Hypertensive crisis: Top number over 180 and/or bottom number over 120, with patients needing prompt changes in medication if there are no other indications of problems, or immediate hospitalization if there are signs of organ damage.
Other changes in the new guideline include:
- Only prescribing medication for Stage I hypertension if a patient has already had a cardiovascular event such as a heart attack or stroke, or is at high risk of heart attack or stroke based on age, the presence of diabetes mellitus, chronic kidney disease or calculation of atherosclerotic risk (using the same risk calculator used in evaluating high cholesterol).
- Recognizing that many people will need two or more types of medications to control their blood pressure and that people may take their pills more consistently if multiple medications are combined into a single pill.
- Identifying socioeconomic status and psychosocial stress as risk factors for high blood pressure that should be considered in a patient's plan of care.
Conclusion:
The revised guideline which defines the High blood pressure as readings of 130 mm Hg and higher for the systolic blood pressure measurement or readings of 80 and higher for the diastolic measurement is a change from the old definition of 140/90 and higher, reflect complications that can occur at those lower numbers. By lowering the definition of high blood pressure, the guidelines recommend early intervention to prevent further increases in blood pressure and the complications of hypertension.
2. Quality of stent procedures consistently good across U.S. regardless of popular hospital ranking
Hospitals ranked amongst the best in Cardiology and Heart surgery by U.S. News and World Report appear no better, at performing percutaneous coronary intervention (PCI), a potentially life-saving heart procedure, than unranked hospitals, according to a preliminary research presented at the American Heart Association's Scientific Sessions 2017, a premier global exchange of the latest advances in cardiovascular science for researchers and clinicians21.
Researchers based their comparison, of PCI results at ranked and unranked hospitals on patient information and PCI outcomes submitted to the National Cardiovascular Data Registry CathPCI. Altogether, researchers reviewed the results of 509,153 angioplasties performed between July 2014 and June 2015 at 654 hospitals (six hospitals ranked among the top 50 by U.S. News and World Report in 2015 were not included in this study because they either did not submit data to the registry or performed an insignificant number of PCIs, making comparisons difficult).
The study found that ranked and unranked hospitals had:
- similar rates of in-hospital deaths (less than 2 percent); and
- similar rates of acute kidney injury and bleeding—two of the most common complications of PCI, which can increase a patient's risk of dying, hamper recovery and lead to longer hospital stays and increased hospital costs.
Conclusion:
The study found out that there was no difference in the quality of stent procedures across the United States, irrespective of popular hospital ranking, which should come as a reassurance to the patients undergoing the percutaneous coronary intervention procedures.
3. Gobbling your food may harm your waistline and heart
People who eat slowly are less likely to become obese or develop metabolic syndrome or a cluster of heart diseases or diabetes and stroke risk factors, according to a preliminary research presented at the American Heart Association's Scientific Sessions 201722.
Metabolic syndrome occurs when someone has any of three risk factors that include abdominal obesity, high fasting blood sugar, high blood pressure, high triglycerides and/or low HDL cholesterol, said Japanese researchers. The researchers evaluated 642 men and 441 women, average age 51.2 years, who did not have metabolic syndrome in 2008. They divided the participants into three groups depending on how they described their usual eating speed: slow, normal or fast.
After five years, the researchers found:
- Fast eaters were more likely (11.6 percent) to have developed metabolic syndrome than normal eaters (6.5 percent) or slow eaters (2.3 percent);
- Faster eating speed was associated with more weight gain, higher blood glucose and bigger waistline.
Conclusion:
Eating more slowly may be a crucial lifestyle change to help prevent metabolic syndrome. The researchers concluded that when people eat fast they tend not to feel full and are more likely to overeat. Eating fast causes bigger glucose fluctuation, which can lead to insulin resistance.
4) Sudden cardiac death rates may be seven times higher among young people with diabetes
Children and young adults with diabetes may be seven times more likely to die from sudden cardiac death compared to children and young adults without diabetes, according to a preliminary research from Denmark presented at the American Heart Association's Scientific Sessions 201723.
Sudden cardiac death is defined as a sudden, unexpected death that occurs instantly or shortly after symptoms appear. It is often caused by malfunctions in the heart's electrical system. The study, which was conducted in Denmark, also found that overall, compared to those without diabetes, children and young adults, ages 1-49, with diabetes were eight times more likely to die from any kind of heart disease, such as heart failure or the chronic narrowing of arteries known as atherosclerosis, compared to children and young adults without diabetes.
Young people with diabetes may be at increased risk of sudden cardiac death because of abnormalities in their blood vessels caused by the disease.
The study is one of the first to examine causes of death and cause-specific death rates among children and young adults with diabetes in a nationwide setting.
The study population consisted of all persons in Denmark age 1 to 35, in 2000-09 and age 36 to 49 in 2007-09. During the 10-year study period 14,294 deaths occurred, and the cause of death was established based on information from death certificates and autopsy reports. The Danish Register of Medicinal Product Statistics, which holds information on all prescriptions dispensed from Danish pharmacies, was used to identify persons with either Type 1 or Type 2 diabetes. Among those who died, 669 (5 percent) had diabetes, of which 471 (70 percent) had Type 1 and 198 (30 percent) had Type 2.
Conclusion:
The study shows the importance of early and continuous cardiovascular risk monitoring in children and young adults with diabetes. In the light of the results from this study, tight control and effective treatment of blood lipids, blood pressure, and blood glucose is also important among children and young persons with diabetes. Healthcare providers need to be aware that even young patients with diabetes have elevated risk of mortality and that this can mainly be explained by increased risk of sudden cardiac death.
5) Men more likely to receive bystander Cardiopulmonary Resuscitation (CPR) in public than women
Men are more likely to receive bystander CPR in public locations compared to women, and they are more likely to survive after the life-saving measure, according to a preliminary research presented at the American Heart Association's Scientific Sessions 201724.
CPR involves pushing on the chest, so it could make people less certain whether they can or should perform CPR in public on women.
The data for the study was compiled by the Resuscitation Outcomes Consortium, a network of regional clinical centers in the United States and Canada that study out-of-hospital treatments of cardiac arrest and trauma, where the researchers analyzed 19,331 cardiac events in the home and in public.
- The preliminary results released showed 45 percent of men received bystander CPR in public settings compared to just 39 percent of women. By the time men were discharged from the hospital, their odds of survival were 23 percent greater compared to women.
- The disparity narrowed to 35 percent of women and 36 percent of men receiving CPR when the emergencies occurred at home. There was no significant statistical difference.
According to the American Heart Association, approximately 90% of individuals who have an out-of-hospital cardiac arrest (OHCA) die; but CPR, especially if given immediately, can double or even triple the chance of survival.
Conclusion:
The study researchers concluded that these findings identify a gap in bystander CPR delivery that can help improve future messaging and training to lay responders, health care providers and dispatchers.
Footnotes
20. https://news.heart.org/nearly-half-u-s-adults-now-classified-high-blood-pressure-new-definitions/
22. https://newsroom.heart.org/news/gobbling-your-food-may-harm-your-waistline-and-heart?preview=1e06
The content of this article is intended to provide a general guide to the subject matter. Specialist advice should be sought about your specific circumstances.

